While your feet may seem like the most grounded part of your body, they’re surprisingly vulnerable to the potential complications of diabetes, and the resulting ulcers can be devastating if left unchecked.
As someone living with diabetes, you’re likely no stranger to the importance of foot care, but understanding the five stages of diabetic foot ulcers is vital for effective management.
From the initial warning signs of an at-risk foot to the potentially catastrophic consequences of gangrene and amputation, recognising the progression of these ulcers is key to preventing long-term damage, and it all starts with knowing when to seek help.
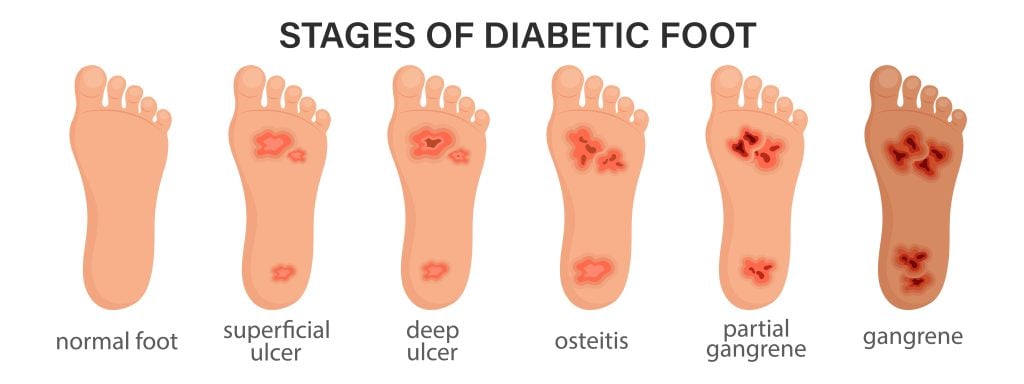
The Five Stages of a Dibetic Foot Ulcer
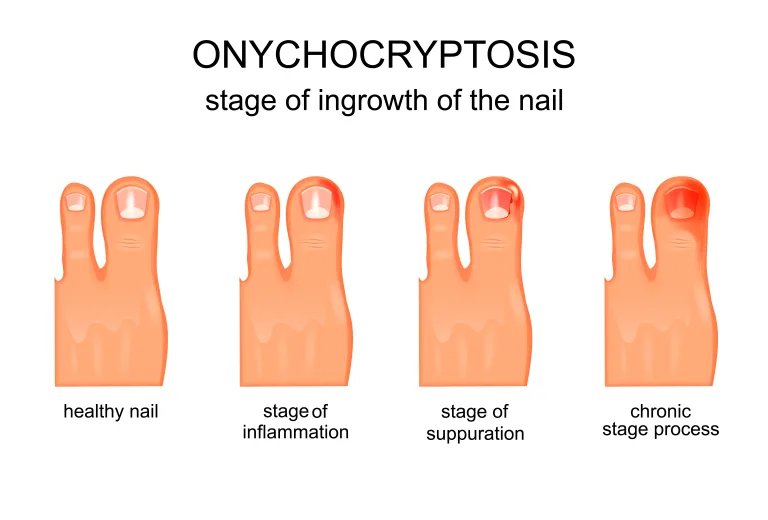
In Stage 1, your foot is considered at-risk due to underlying factors such as nerve damage or reduced blood flow, which increase its vulnerability to developing ulcers, even if no visible signs of ulcers or infections are present. This stage is pivotal in the development of a diabetic foot ulcer, and it’s essential that you take preventive measures to avoid progression.
You may not experience any pain or discomfort, which is why regular foot exams are crucial for early identification.
As someone with an at-risk foot, you’re more likely to develop ulcers due to nerve damage or reduced blood flow. This highlights the importance of maintaining excellent blood sugar control and wearing appropriate footwear to prevent ulcers.
Early detection and intervention can markedly reduce the risk of complications. By taking proactive steps, you can prevent the development of a more severe ulcer.
Don’t underestimate the value of preventive measures at this stage. By controlling your foot health, you can enjoy the freedom to live an active life without the burden of a diabetic foot ulcer.
At a pivotal juncture in the progression of a diabetic foot ulcer, Stage 2 marks the actual formation of an open wound on your foot, typically resulting from compromised blood flow or nerve damage in the affected area.
This stage signifies a turning point in the disease’s progression, and prompt action is necessary to prevent further complications. If you have diabetes mellitus, it’s crucial to inspect your feet regularly for signs of trouble, such as blisters, cuts, or discoloration.
During Stage 2, you may notice a breakdown in tissue, leading to the formation of a foot ulcer. Pressure, trauma, or neuropathy can cause this. Seeking professional help from a podiatrist is vital at this stage. They can provide diabetic foot ulcer treatment, including wound care and management, to promote healing and prevent the ulcer from progressing to more severe stages.
Stage 3 of a diabetic foot ulcer typically marks a pivotal turning point, where the ulcerated area becomes infected, significantly increasing the risk of complications if left untreated or poorly managed.
At this stage, you’ll likely notice signs of infection, such as redness, warmth, and swelling around the ulcer. It’s vital to seek medical attention promptly to prevent the infection from spreading further and causing more severe issues.
If you’ve reached Stage 3, your healthcare provider may prescribe antibiotics to treat the infection and prevent it from worsening. Take the full course of antibiotics as prescribed to ensure complete clearance of the infection.
Without proper treatment at Stage 3, the ulcer can progress to more advanced stages, potentially leading to serious consequences like tissue damage or amputation. Don’t hesitate to seek professional help if you notice any signs of infection or if your ulcer isn’t healing.
Early intervention can make a significant difference in preventing long-term damage and preserving your mobility and independence. Take action now to reduce your risk of complications and promote healing.
When your diabetic foot ulcer progresses to the point where blood flow is severely compromised, you’re at risk of developing foot gangrene, a severe complication characterised by the death of tissue in the affected area. Foot gangrene is a serious condition that necessitates immediate medical attention to prevent further tissue damage and potential amputation.
As gangrene develops, you may notice blackened, dry, and shrivelled skin in the affected area. This is a sign that the tissue has died due to a lack of blood flow. If left untreated, gangrene can spread quickly, leading to severe consequences.
Here are three key things to know about foot gangrene:
- Gangrene can happen quickly. It can develop in a matter of days, so it’s crucial to monitor your foot ulcer closely for any signs of trouble.
- Gangrene requires immediate medical attention. If you suspect you have gangrene, seek help right away to prevent further tissue damage.
- Treatment may involve surgery: Your doctor may need to surgically remove dead tissue to prevent the spread of gangrene and promote healing.
Severe diabetic foot ulcers often culminate in Stage 5, where the risk of amputation becomes a harsh reality, calling for immediate medical intervention to prevent further complications and promote recovery. Infected with gangrene, amputation may be the only way to stop the spread of infection and save your life. You’ll require careful evaluation and treatment by a multidisciplinary team of healthcare professionals to determine the best course of action.
If amputation is necessary, your recovery will involve rehabilitation, prosthetic fitting, and lifestyle adjustments to regain mobility and independence. You’ll need ongoing medical support, physical therapy, and emotional counselling to cope with the emotional and physical challenges of amputation. It’s crucial to collaborate closely with your healthcare team to guarantee proper wound care and prevent complications.
With the right treatment and support, you can adapt to your new circumstances and maintain a satisfactory quality of life.
When to Seek Professional Help For Your Diabetic Foot
If you have diabetes and develop a foot ulcer, it’s essential to seek medical attention promptly to prevent complications and promote proper healing. Delaying treatment can lead to infections, amputations, and even life-threatening complications.
You should be vigilant about monitoring your condition and seek professional help when necessary.
Here are the key signs that indicate when to seek help:
- Increased redness, warmth, or swelling: These symptoms can indicate an underlying infection that requires immediate treatment.
- Persistent pain, foul odour, or discharge: These signs can point to a more severe complication that needs prompt medical care.
- No signs of healing or increased pain: If your foot ulcer shows no signs of improvement after a few days or hurts more, you should schedule an appointment with your podiatrist.

Frequently Asked Diabetic Foot Questions...
-
When Should I Go to the ER for a Diabetic Foot Ulcer?
You should go to the ER for a diabetic foot ulcer if you notice severe symptoms. Seek immediate attention if you experience persistent pain, a foul odor, or drainage from the ulcer.
Additionally, if you notice black tissue, dead skin, or numbness spreading beyond the ulcer, or if you have a fever, chills, or systemic symptoms, don't delay - head to the ER to prevent severe complications like gangrene or amputation.
-
How Serious Is a Diabetic Foot Ulcer?
You're likely underestimating the severity of a diabetic foot ulcer. It's a serious condition that can lead to infections, gangrene, and even amputations if left untreated.
In fact, 14-24% of patients with diabetes who develop a foot ulcer require an amputation.
Don't delay seeking medical attention if you notice signs of trouble, such as pain, swelling, or redness. Prompt treatment can prevent severe consequences and preserve your freedom to live an active life.
-
What Is the Management Plan for Diabetic Foot Ulcer?
Taking the reins of your diabetic foot ulcer management is a 'step in the right direction.' You'll need to inspect your feet daily, reporting any changes to your doctor. Your treatment plan will include:
- wound care
- debridement
- pressure offloading
You may also need antibiotics or surgery. Don't forget to prioritize blood glucose management and wear suitable shoes to prevent further complications. Regular check-ups are key to staying on the path to healing.
-
Should You Elevate a Diabetic Foot Ulcer?
You should consider raising a diabetic foot ulcer to reduce swelling and improve blood flow. Elevate your foot above heart level for 15-20 minutes, several times a day.
However, avoid prolonged periods of sitting with legs crossed, which can restrict blood flow.
Before starting an elevation routine, consult with your healthcare professional to make sure it's suitable for your specific case, as individualized advice is essential for effective management.
Diabetic Foot Conclusion...
You’ve navigated the five stages of diabetic foot ulcer progression, from an at-risk foot to the potential need for amputation and recovery.
Think of your foot health as a ship sailing through treacherous waters—prompt attention to early warning signs can prevent catastrophic damage. Regular inspections and swift consultation with podiatrists are your anchors, holding you secure against the tide of complications.
Seek assistance whenever necessary to prevent becoming overwhelmed.
Know your risk – a short 30 minute consult could save your feet.
Book in today to see one of our experienced Podiatrists, call us on (03) 4237 7165 or book online for a GAP FREE Diabetes Foot Health Assessment (or just $59 if no extras cover).
Diabetic Foot
Understand what diabetes means for your feet and make sure you know the steps to protect your foot health long term. Learn how to avoid unnecessary foot health complications to keep your feet and toes healthy for life.


Bellevue Podiatry
Bellevue Podiatry has been serving the people of Rosanna and its surrounding suburbs for over 10 years. We have the qualifications, experience and education to effectively treat any lower limb condition or injury that requires expert podiatry care.
Diabetic Feet Care Article References:
If you would like to know more about diabetic foot ulcers, please feel free to click on the links below to read more from the sources we referenced to write this blog:
Mayo Clinic: https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-minute-5-steps-to-diabetic-foot-care/
Healthline: https://www.healthline.com/health/diabetic-foot-pain-and-ulcers-causes-treatments
American Diabetes Association: https://diabetes.org/health-wellness/diabetes-and-your-feet/foot-care-tips
Centers for Disease Control and Prevention: https://www.cdc.gov/diabetes/communication-resources/diabetes-foot-problems-when-to-see-your-doctor.html
Cleveland Clinic: https://my.clevelandclinic.org/locations/mercy-hospital/specialties/diabetes-education
Podiatry Learning Network: https://www.hmpgloballearningnetwork.com/site/podiatry/blog/preventing-next-generation-foot-ulcers-and-amputations
Wound Source: https://www.woundsource.com/blog/preventing-diabetic-foot-ulcers-through-regular-foot-checks