When exploring the top compression socks for 2025, you’ll encounter a range of advanced options designed to optimise circulation and comfort.
These selections use clinical insights and evidence-based support to cater to various needs, from enhancing athletic performance to alleviating circulation issues in sedentary individuals. Any choice offers features like specific compression levels, durable materials, and cooling benefits, promising long-term effectiveness.
Want to know more about how these can enhance daily performance or recovery? Please read our latest blog to learn more.
Key Takeaways
- Copper-infused knee-high compression socks provide cooling technology, which is ideal for athletes and travellers seeking comfort.
- EvoNation Compression Socks offer 20-30 mmHg compression, perfect for circulation issues and long-standing hours.
- TechWare Pro Sleeve supports recovery from plantar fasciitis with firm compression and versatile design.
- Fenglaoda Socks maintain quality compression after many washes, which is ideal for conditions like POTS and primary lymphedema.
- CHARMKING Compression Socks with 15-20 mmHg compression cater to athletes, office workers, and seniors for enhanced circulation.
Copper-infused Knee High Athletic Performance Cooling Socks (2 Pack) offer an innovative solution for athletes and frequent travellers who demand both function and comfort. These compression socks integrate patent-pending cooling technology to regulate foot temperature by dissipating heat effectively. You’ll appreciate the advanced moisture-wicking fabric that ensures sweat control, preventing irritation. The copper infusion preserves freshness, making them ideal for continuous wear.
Gentle compression socks facilitate peak blood circulation, which is essential for reducing fatigue and enhancing performance. Users consistently report satisfaction with Coppsox’s comfort and effectiveness, particularly in demanding environments, making them a compelling choice for anyone seeking reliable, high-performance compression socks.

For those seeking reliable compression and comfort, particularly individuals with circulation issues or who spend long hours on their feet, EvoNation Men’s Knee High Graduated Compression Socks (20-30 mmHg) stands out as an effective solution.
Despite some fit and sizing challenges, these compression socks generally deliver desirable compression and enhance venous return, alleviating swelling.
Users frequently commend their comfort and report feeling rejuvenated post-use for their compression socks. While some experience constriction at the ankle, durability aligns well with expectations when maintained correctly.
Offering excellent value, they often outperform pricier alternatives. Praised customer service and compelling benefits result in continued purchases and recommendations.
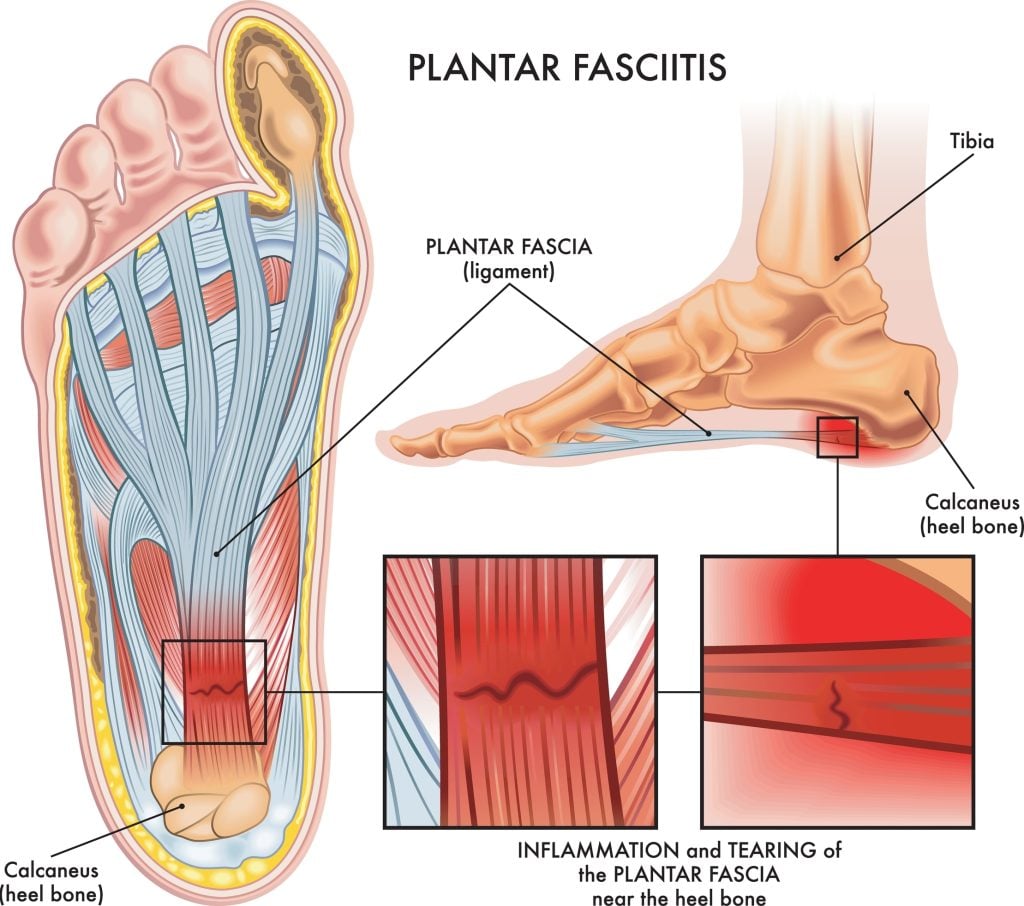
The TechWare Pro Ankle Brace Compression Sleeve is an ideal choice for individuals with Achilles tendonitis, joint pain, or plantar fasciitis.
Made from 80% nylon and 20% spandex, its lightweight, breathable design supports arthritis, sprains, muscle fatigue, and stress fractures. You’ll experience fast relief from plantar fasciitis, as it supports the heel and arch, reducing inflammation and promoting recovery.
These compression socks enhance circulation and stability, making them suitable for running, hiking, or tennis activities.
Accurate sizing is essential, as reports indicate it can fit snugly, though some experience sliding or irritation during extended wear.
Delivering robust compression, Fenglaoda Compression Socks at 20-30 mmHg is an ideal choice for individuals managing conditions like POTS and primary lymphedema, requiring therapeutic daily use.
These compression socks offer significant relief with better circulation compared to lower-grade options. You might initially experience mild itchiness due to enhanced microcirculation, which is standard with low baseline circulation.
Selecting the right size is essential—size S/M is best if you’re 5’7″ with 16″ calves. Despite muscular legs, the fit is adept without constriction. The fabric remains durable and practical after many washes, while the vibrant colours enhance aesthetics and lift moods. Consider these compression socks for reliable compression and extended comfort.
Boasting a compression level of 15-20 mmHg, CHARMKING Compression Socks cater to athletes, office workers, pregnant women, and seniors seeking enhanced circulation and comfort.
These compression socks comprise 85% nylon and 15% spandex and ensure flexibility, durability, and breathability.
Clinical insights show these compression socks effectively promote blood circulation and oxygen flow, preventing fatigue and aiding muscle recovery. Trainers recommend them for reducing swelling.
They fit snugly yet comfortably, measuring 8.43 x 4.25 x 2.64 inches and weighing 0.25 kg. Despite limited style options, users report high satisfaction with comfort and support. Ranked highly in sales, they’re a best-seller choice for compression socks.
When you’re seeking both comfort and improved circulation, FuelMeFoot Copper Compression Socks are an excellent choice, especially for those balancing medical needs with everyday activities.
Engineered for both men and women, these compression socks offer superior compression, enhancing blood flow and reducing lower-limb edema.
The stretchy, breathable fabric ensures a snug yet comfortable fit, effectively maintained across activities like running or extended sitting.
Although sizing for larger feet can be tricky, adhering to the size chart mitigates this issue.
Enhanced durability allows repeated washing without losing functionality, guaranteeing consistent performance and making them a reliable, value-packed selection.

If you’re seeking ideal circulation and comfort, CHARMKING Compression Socks for Women & Men offer a perfect solution with their 15-20 mmHg compression level. Clinical research recognises this prime range for its ability to enhance speed, elevate energy efficiency, and support various daily activities through targeted compression zones.
Crafted from 85% nylon and 15% spandex, these compression socks guarantee a snug yet comfy fit. Users benefit from the breathable fabric’s 360-degree stretchability, assuring temperature regulation and ease of wear. Tailored for athletes and professionals, these socks excel in alleviating swelling, promoting circulation, and providing long-term support, validated by overwhelmingly positive feedback.
Fenglaoda Compression Socks, offering a robust 20-30 mmHg compression, is an excellent choice for those managing POTS or primary lymphedema and requiring daily compression wear. They’re designed to enhance venous return, thereby alleviating symptoms associated with circulatory deficiencies.
Shifting from 15-20 mmHg compression socks, you’ll notice an improved compression profile with these socks, notwithstanding the mild itchiness due to increased circulation. The size S/M accommodates calves up to 16″ and 9.5″ ankles effectively, ensuring a comfortable yet secure fit. Durable and vibrant, Fenglaoda socks are suited for travel and daily activities, providing lasting efficacy even with frequent washes.
Factors to Consider When Choosing Compression Stockings / Socks
When selecting compression socks, prioritise the compression level range, as matching the therapeutic pressure with your specific needs is vital. Proper sizing and fit are essential to maximising clinical efficacy and preventing discomfort, so consult sizing charts and consider professional fitting if necessary.
Evaluate material composition, breathability, and durability to guarantee long-term wear and easy maintenance while balancing comfort and functionality.
Compression Level Range
Selecting the right compression level for your compression socks is crucial for maximising their benefits while ensuring comfort. Compression socks typically range from 15-20 mmHg for mild support to 20-30 mmHg for moderate to firm support, addressing various circulatory needs.
For general use, such as minimising fatigue and minor swelling, a 15-20 mmHg compression is advisable, making them practical for athletes and sedentary office workers. Conversely, severe conditions like POTS and lymphedema often utilise higher levels like 20-30 mmHg, offering substantial circulatory assistance.
It’s essential to choose compression socks based on your health requirements; insufficient pressure might not be adequate, whereas excessive pressure could lead to discomfort. Initial tingling or itchiness is familiar and typically related to enhanced circulation.
Sizing and Fit
Even though choosing compression socks may seem straightforward, ensuring the correct size and fit is crucial for their effectiveness. Accurate sizing is essential; a poorly fitting sock can lead to inadequate compression or excessive constriction. To achieve the best fit, accurately measure your foot size and calf circumference using brands’ sizing charts as a guide.
This data helps correlate your measurements to appropriate sock sizes. Compression levels, such as 15-20 mmHg or 20-30 mmHg, should match your specific circulatory needs. It’s essential to avoid variability in fit, as sizes can run large or small based on styles, so review customer feedback. Properly fitted compression socks should feel snug, enhancing comfort and promoting adequate blood circulation during extended wear.
Material Composition
Understanding the material composition of compression socks is key to maximising their therapeutic benefits and ensuring your comfort. These compression socks typically blend nylon and spandex, forming the backbone of elasticity and longevity.
High nylon content, around 85%, is advantageous for enhancing breathability and moisture-wicking capabilities, which are vital for maintaining comfort during prolonged use. Meanwhile, spandex, usually constituting 15-20% of the fabric, is essential in preserving the compression socks shape and providing effective compression, necessary for adhering to therapeutic pressures like 15-20 mmHg or 20-30 mmHg.
Premium material blends often exhibit superior stretch and recovery properties, preventing sagging and compression loss. Additionally, tailored combinations of these materials can streamline applications, especially for high-compression variants.
Summing It Up...
When looking for the best compression socks, how do you choose between options like Copper Infused or EvoNation’s 20-30 mmHg solutions? Consider the specific compression levels you need for ideal circulation and recovery.
Don’t overlook material durability and breathability to guarantee long-term effectiveness, even after numerous washes. Whether you’re an athlete or have circulation concerns, these compression socks offer targeted benefits. Ultimately, choosing the right compression socks directly impacts your circulation and comfort.

Bellevue Podiatry Treatment Clinic
Bellevue Podiatry has been serving the people of Rosanna and its surrounding suburbs for over 10 years. We have the qualifications, experience and education to effectively treat any lower limb condition or injury that requires expert podiatry care.

Nicole Hardidge - Principal Podiatrist
Nicole graduated with a Bachelor of Podiatry from Latrobe University in 2009 with a certificate in Advanced Clinical Education. Nicole has completed her post graduate certificate in wound care through Monash University.