Imagine reducing foot pain, rediscovering mobility, and enhancing quality of life, all with just a pair of shoes. Orthopedic shoes have evolved significantly from bulky designs, incorporating biomechanical engineering and clinical data to enhance foot support and comfort.
In 2024, top contenders like Skechers and Orthofeet elevate this standard with innovative cushioning technologies and adaptive fit systems. But which shoe aligns with your specific foot needs? Whether memory foam insoles or slip-resistant outsoles, these shoes address more than style. So, what factors should you consider when redefining foot health this year?
Key Takeaways
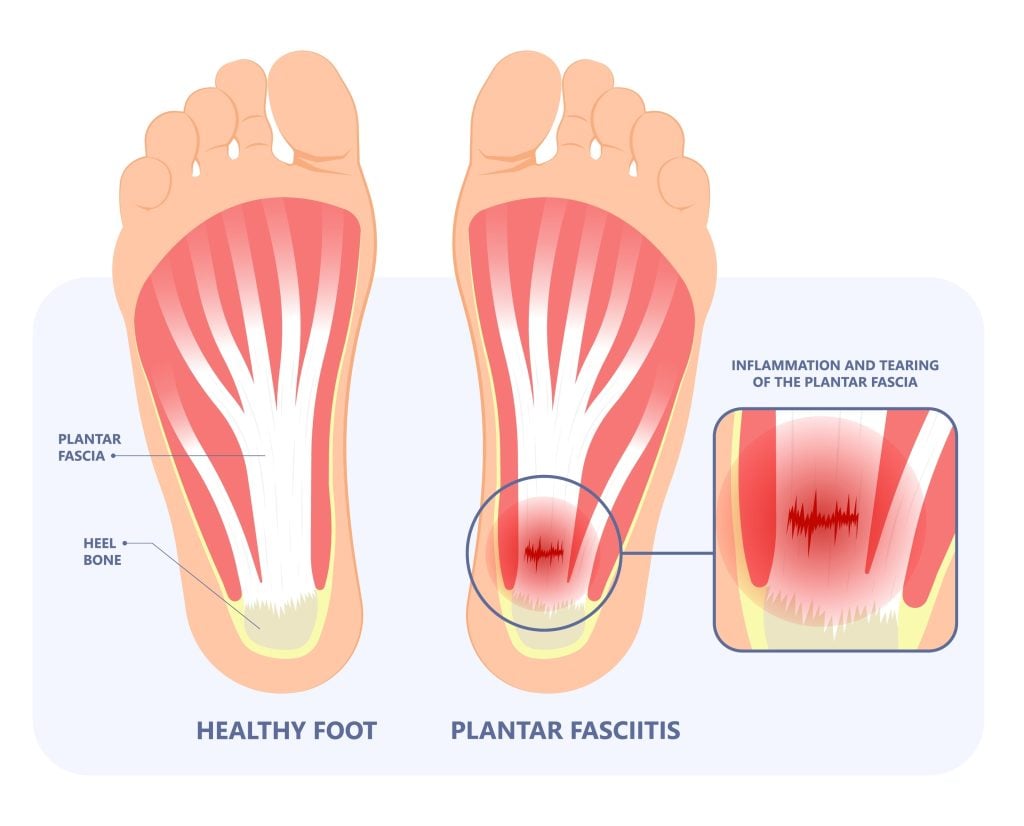
- OrthoComfoot Men's Loafers offers engineered arch support and ergonomic design to relieve plantar fasciitis and heel pain.
- Skechers Women's Uno Sneakers provide wide-width options, water resistance, and excellent reviews from healthcare workers for superior comfort.
- The Orthofeet Women's Winter Boot combines a waterproof design with orthotic footbeds for great arch support and excellent traction on icy surfaces.
- STQ Women's Lace-up Loafers feature stretchy materials and slip-resistant soles for wider feet and diverse activities.
- Goga Max Slip-On Shoes utilize a high-rebound insole with a breathable mesh upper for customization and lightweight support.
If you’re looking for orthopedic shoes that combine functionality with comfort, the OrthoComfoot Men’s Orthopaedic Slip-On Loafers with Arch Support provide an excellent solution. These shoes deliver well-engineered arch support, essential for mitigating plantar fasciitis and heel pain. Users have reported exceptional ease of use as the slip-on design facilitates easy wearing and secure grip, enhancing daily usability.
Although some experience initial tightness, the expectation is that it gradually moulds to your foot, offering adaptive comfort. Objective feedback suggests their ergonomic design aligns with foot anatomy, reducing strain during prolonged activities. It’s notable that while traction issues on wet surfaces exist, the overall benefits outweigh this limitation. Recurrent purchases underscore their perceived value and continuous user satisfaction, confirming their support efficacy.

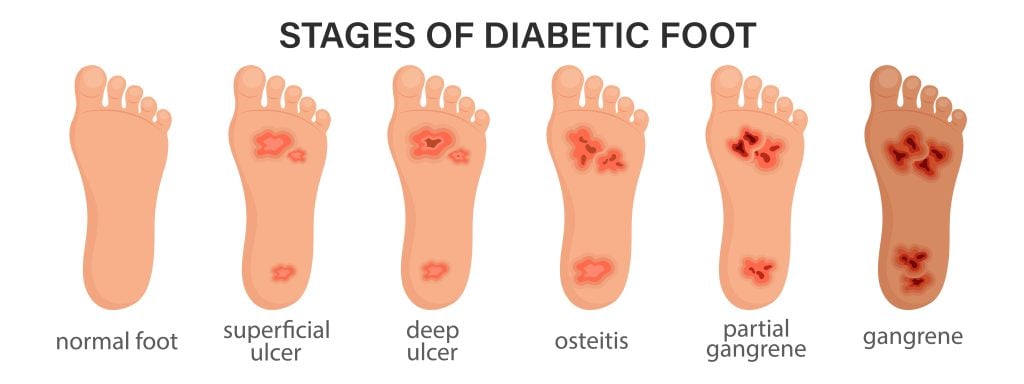
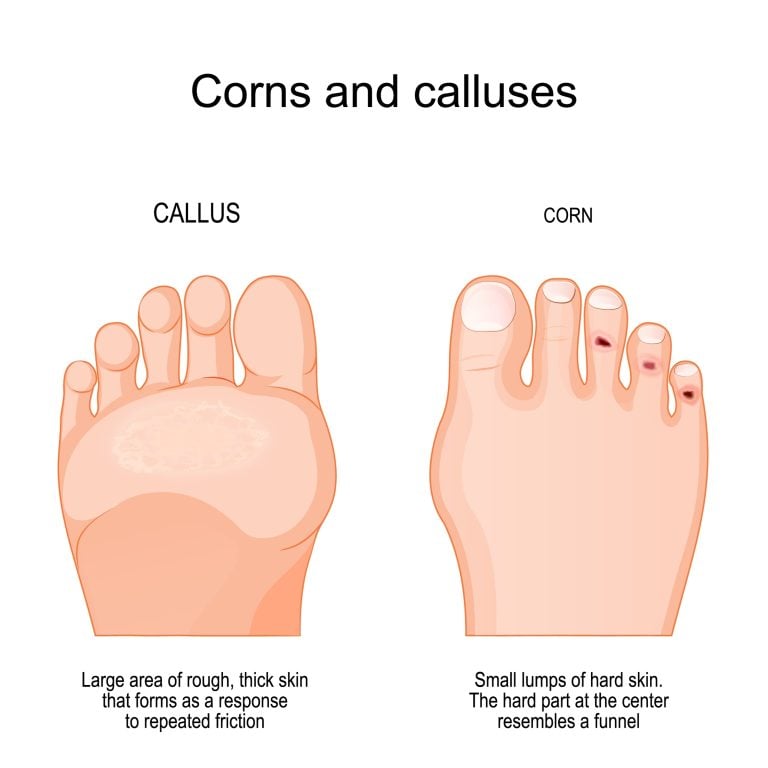
STUNAHOME Orthopaedic Women’s Walking Shoes are an excellent choice for individuals seeking reliable comfort and support during extended periods of walking or standing. Customers frequently commend these shoes for their durable construction and high comfort levels, essential for mitigating foot fatigue and ensuring musculoskeletal health. However, consider sizing adjustments for best fit, especially if accommodating specific foot conditions like ingrown toenails.
While some users report durability and comfort issues, including blisters and lack of cushioning, the majority highlight the materials’ softness. People praise the shoes’ aesthetic appeal despite design challenges that complicate donning. Evaluation of pressure distribution and shock absorption features is vital, as these influence long-term foot health and injury prevention in active settings.
HKR Women’s Walking Shoes with Arch Support is an excellent choice for individuals requiring both comfort and orthopaedic benefits, particularly those experiencing flat feet or chronic heel pain. These shoes integrate memory foam construction with a supportive arch insole, offering significant relief from heel discomfort. Their breathable, stretchable fabric guarantees the feet remain dry and comfortable during extended wear, which is vital for mitigating foot pain. The lightweight design and slip-resistant rubber outsole enhance stability, making them suitable for various environments. Customer testimonials affirm the alleviation of foot pain during activities, attesting to the shoe’s functional capabilities. Aesthetically, the shoes offer diverse colours with a sleek design, appealing to those seeking both style and adequate orthotic support.
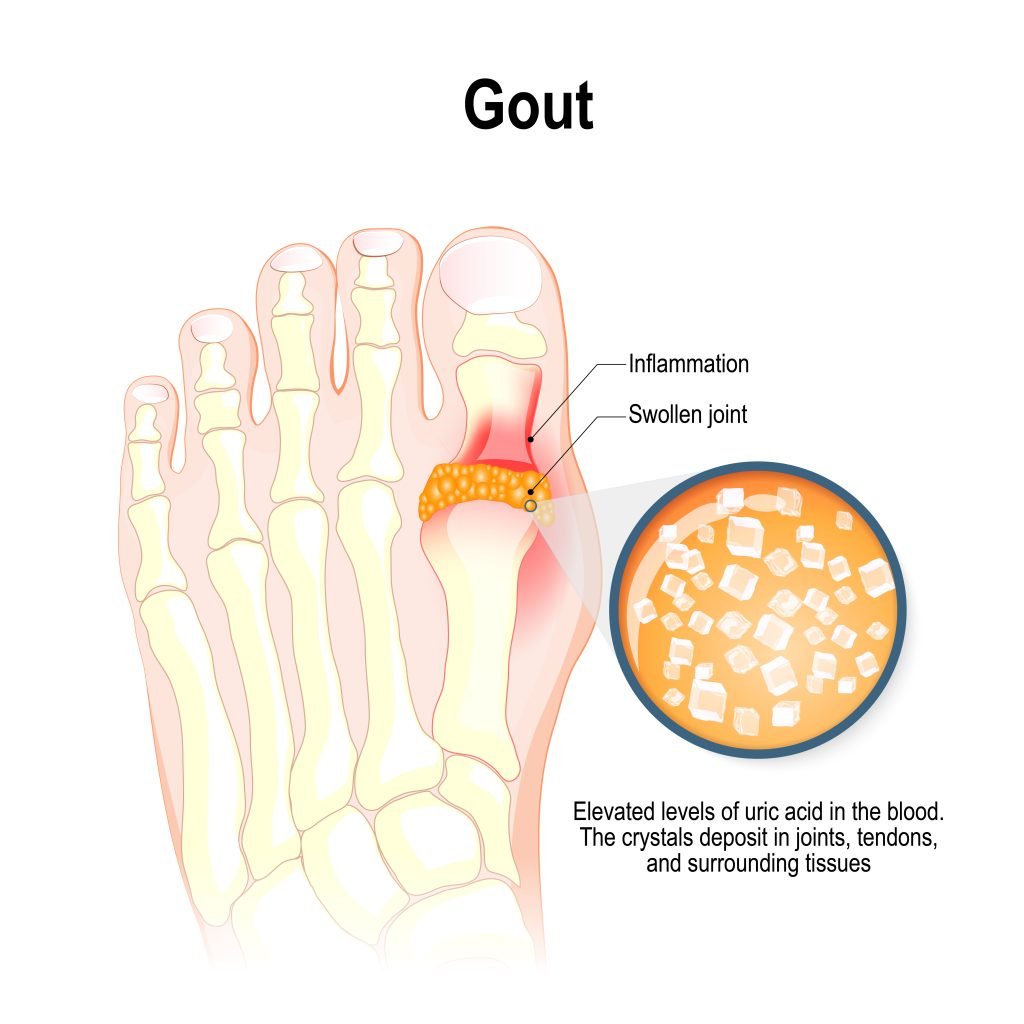
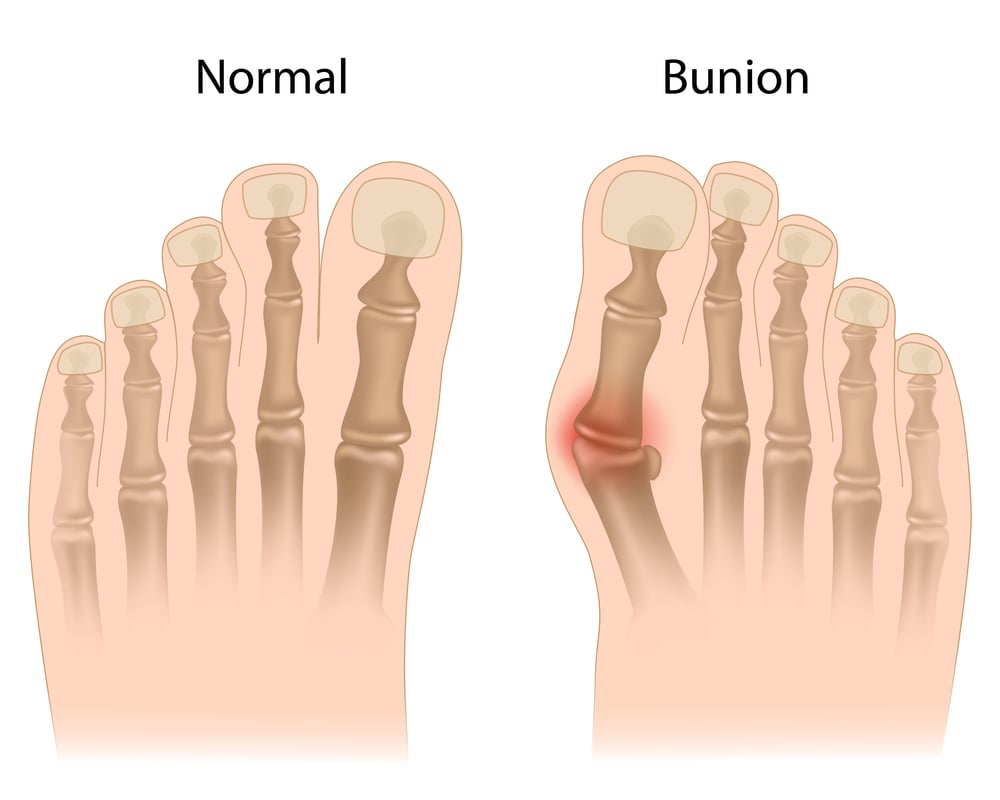
For those seeking orthopaedic support with a touch of style, the Skechers Women’s Uno Stand-On Air Sneaker stands out. Their durable and non-slip features accommodate orthopaedic insoles, making them ideal for prolonged standing or walking. A key advantage is the wide-width option, easing discomfort from bunions, and the higher heel design that aids back support. Healthcare workers have positively reviewed them, highlighting effective orthopaedic interventions in daily routines.
Some users report initial discomfort but recommend breaking in the shoes for the best fit. Pricing is reasonable, correlating with high quality and sufficient cushioning. For flat feet or lower back pain relief, consider additional inserts. The water-repellent quality, ease of maintenance, and colour flexibility appeal to varied lifestyle needs.
STQ Women’s Orthopaedic Lace-up Loafers might be the ideal choice when searching for orthopaedic footwear that combines aesthetics with functionality. Unlike generic options like Hey Dudes, these loafers provide superior arch support, delivering a lightweight and ergonomic design. The stretchy material is especially beneficial for individuals with wider feet and guarantees a comfortable fit for all-day wear. The design meets the biomechanical requirements necessary for reducing foot strain and enhancing both comfort and utility.
From a value perspective, STQ offers an affordable option without compromising quality. Their durable construction includes slip resistance, supporting various activities from concrete walking to deep-sea fishing. Although some users suggest additional arch support inserts, the overall feedback highlights repeat purchases and favourable durability, indicating a trustworthy investment in orthopaedic footwear.

Delivering unmatched comfort, the Skechers Men’s Go Walk Max Effort is a superb choice for individuals seeking orthopedic shoes with strong support in 2024. The Goga Max high-rebound insole ensures optimal shock absorption and energy return, which is essential for reducing musculoskeletal strain during extended activities. The lightweight construction and breathable mesh upper of the insole aid in thermoregulation, reducing sweat and subsequent foot irritation. The slip-on style with a stretchy collar enhances user accessibility, while the customizable lace-up design caters to personalized fit needs, particularly for wide and tall feet.
Critically, the durable outsole affords exceptional traction, mitigating fall risks—a critical orthopaedic consideration. Its affordability and ease of care enhance its appeal. User feedback underscores its long-distance comfort and minimal chafing, highlighting its efficacy for daily ambulation and errands and invariably confirming its ergonomic design.
Consider the Orthofeet Women’s Orthopaedic Waterproof Winter Boot with Arch Support if you’re looking for superior comfort and support, particularly ideal for individuals with arthritis or other foot ailments. This boot features orthotic footbeds designed to alleviate pain and enhance foot biomechanics.
The architecture includes a comfy heel and robust arch support, essential for distributing weight evenly and minimizing stress on the lower extremities. Made from camel suede, it provides waterproof protection and warmth with a fleece lining, making it perfect for cold climates. Moreover, the boot’s velcro straps allow for an adjustable fit, accommodating swollen feet and ankles. The thick sole offers excellent traction on icy sidewalks, reducing fall risk. Its design merges functionality with style, making it suited for daily wear.
Women’s Woven Orthopaedic Walking Shoes with Arch Support are ideal for those seeking affordable, breathable footwear for light activities or casual outings. User reviews highlight comfort and lightweight features, though sizing discrepancies arise frequently. It’s advisable to size up or add orthopaedic inserts to enhance arch support, as the shoes alone may not be sufficient for prolonged standing or demanding activities.
Despite the anti-slip sole claiming efficacy, structural support is lacking, particularly in the woven upper, which offers minimal elasticity. These shoes could suit low-impact use, like driving or lounging, rather than long-distance walking. The price reflects its basic construction, so if medical-grade support is essential, consider upgrading with custom orthotics. Stay mindful of your fitness to prevent discomfort or slippage.
Summing It All Up...
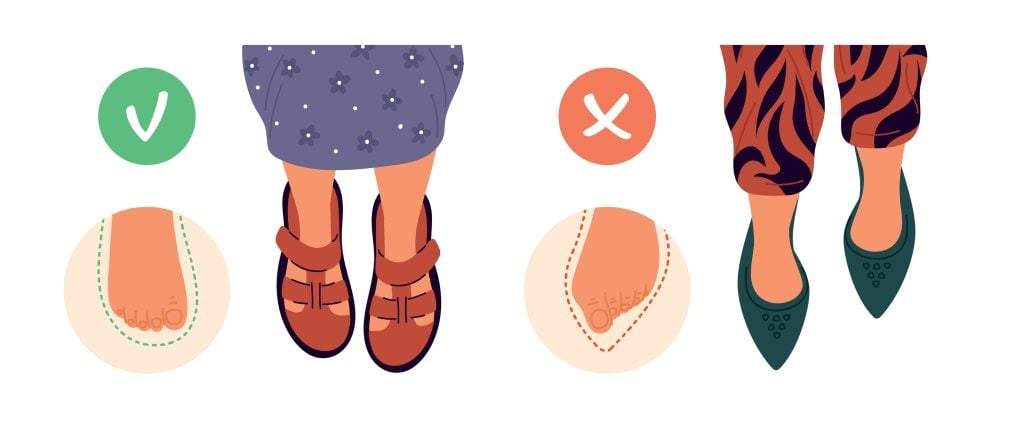
When selecting orthopedic shoes, prioritize features like arch support, cushioning, and slip resistance. Some might think orthopaedic shoes compromise style, but brands like Skechers and Orthofeet prove otherwise by blending aesthetics with advanced technology.
Pay attention to these options due to outdated stereotypes. The recommended shoes provide comfort and support and technical innovations that cater to various foot conditions. Investing in the proper pair guarantees enhanced mobility and overall foot health.

Bellevue Podiatry
Bellevue Podiatry has been serving the people of Rosanna and its surrounding suburbs for over 10 years. We have the qualifications, experience and education to effectively treat any lower limb condition or injury that requires expert podiatry care.