Dealing with an ingrown toenail can feel like a never-ending struggle, but Epsom salt might just be your saving grace if it’s not too late. You’ll find that soaking your foot in a warm Epsom salt solution can offer significant relief for people in the early stages of an ingrown toenail.
Begin by dissolving the salt in a basin of warm water and soaking your foot for about 15–20 minutes twice daily. But don’t get too comfortable—knowing when to seek professional help is equally essential, especially if signs of infection or severe symptoms arise.
Are you unsure about how to effectively strike a balance between home care and professional intervention? Let’s discuss this important distinction further in our latest blog.
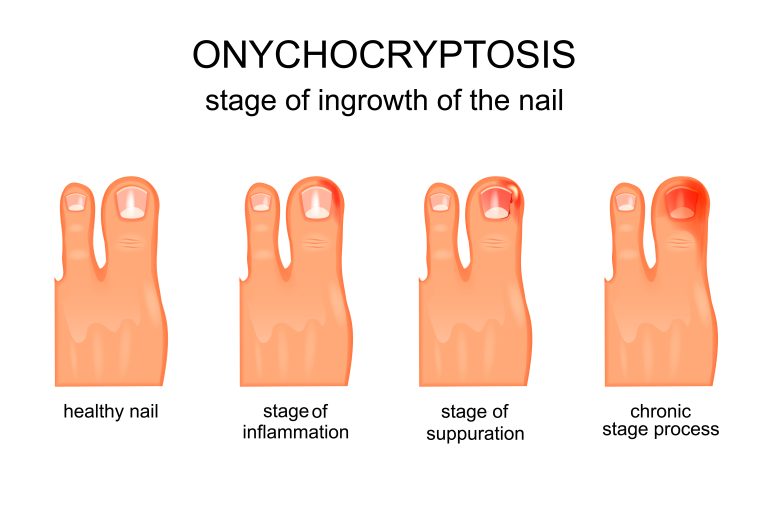
Understanding Ingrown Toenails & If You Need Professional Ingrown Toenail Medical Care
Understanding ingrown toenails begins with recognising that they occur when the toenail’s edge grows into the surrounding skin, causing pain and swelling.
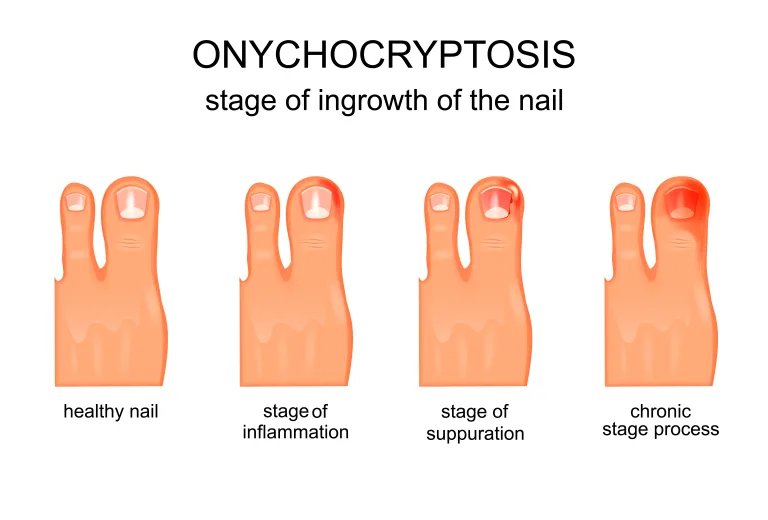
You might notice ingrown toenail symptoms such as redness, tenderness, and a sore big toe nail.
Sometimes, the area can develop an ingrown toenail infection, indicated by increased swelling, pus, and warmth.
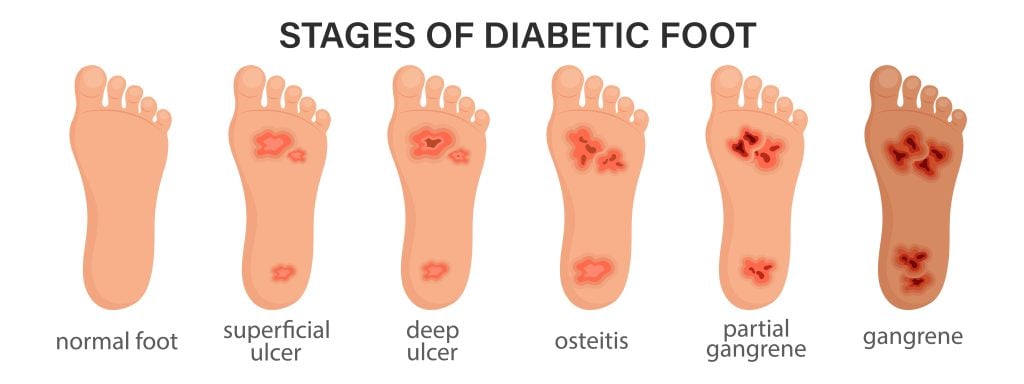
If left untreated, a mildly ingrown toenail can escalate, leading to an infected big toe. Individuals with diabetes or poor circulation are particularly vulnerable and should seek regular podiatrist visits.
An infected big toe can lead to severe complications, so closely monitoring the condition and not delaying professional care if symptoms persist or worsen is crucial for your ingrown toenail.
Epsom Salts Ingrown Toenail Benefits
When dealing with an ingrown toenail, incorporating a foot soak with Epsom salt into your foot care routine can reduce inflammation and enhance circulation in the affected area.
The benefits of using a foot soak with Epsom salt for ingrown toenails issues are positive:
- Reduces inflammation: Epsom salt decreases swelling and redness.
- Improved Circulation: Enhanced blood flow aids in faster healing.
- Natural Pain Relief: Warm foot soaks with Epsom salt alleviate discomfort.
- Antiseptic Properties: Aids in preventing infections around the ingrown toenail.
Step-by-Step Epsom Salts Ingrown Toenail Soak Guide
To start your Epsom salt soak:
- First fill a basin with warm water and dissolve 1-2 tablespoons of Epsom salt thoroughly. Make sure the water isn't too hot to avoid scalding.
- Submerge your affected foot in the basin, ensuring that the water completely covers the ingrown toenail.
- Soak for 15-20 minutes, allowing the Epsom salt to reduce inflammation and soften the skin. This process helps ease pain and improve blood circulation.
- After the soak, gently pat your foot dry with a clean towel. Repeat this soaking routine twice a day for best results.
If you notice any signs of infection or worsening symptoms, seek professional medical advice immediately.
Post Epsom Salts Ingrown Toenail Soak Care Tips
After completing your Epsom salt soak, it’s essential to dry the area thoroughly to prevent moisture-related infections. This step is ideal for minimising the risk of bacterial or fungal growth.
Follow these post-soak care tips:
- Apply a thin layer of antibacterial or antifungal cream to the affected toe to safeguard against infections.
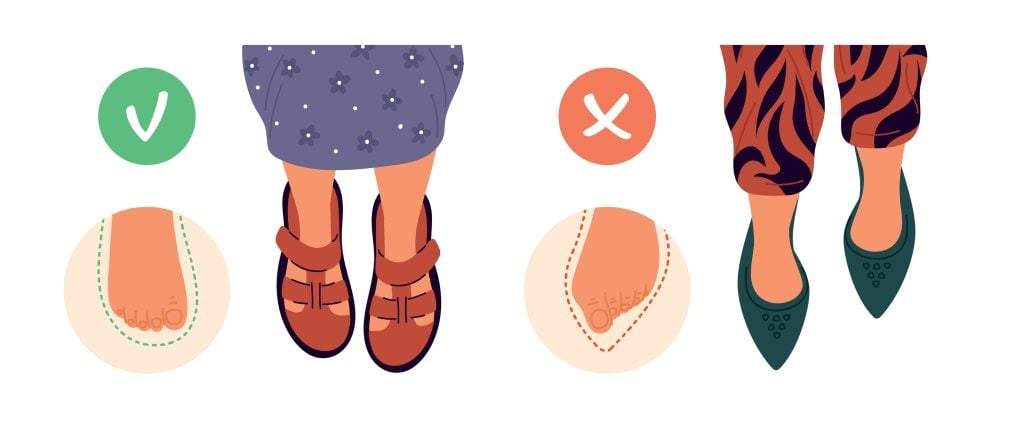
- Avoid wearing tight or constricting footwear to allow the toe to breathe and heal properly.
- Keep the toenail area clean and dry post-soak to promote the best healing and prevent further complications.
- Monitor the ingrown toenail for any signs of worsening infection or discomfort, and seek professional help if necessary.
When to Seek Professional Podiatry Care When Epsom Salt Does Not Work
Persistent pain or signs of infection, such as pus or red streaks, should prompt an immediate consultation with a podiatrist.
If Epsom salt soaks haven’t improved your ingrown toenail after a week, don’t delay. Diabetics or those with circulation issues must act swiftly, as infections can escalate quickly.
Severe symptoms like swelling, fever, or difficulty walking indicate a need for professional evaluation. Podiatrists can offer targeted treatments, including minor surgical procedures or nail removal, to prevent complications.
Ignoring these signs increases the risk of worsening the condition and causing long-term damage. For persistent or worsening symptoms, seeking immediate podiatry helps secure your freedom from prolonged pain and potential severe infections.

Summing It Up...
So, there you have it! You’re now a pro at soaking your ingrown toenails in Epsom salt, as if they were little spa guests. Don’t forget to dry them off and pamper them with cream.
If your toe starts acting like a drama queen with swelling or fever, ring up a podiatrist ASAP. And remember, diabetics, don’t play around with potential danger—get professional help before things spiral out of control.
Your toes will thank you!
If you think you may have an ingrown toenail and want the right professional advice on how to treat it, we currently have a limited offer running to help you out. A GAP FREE ingrown toenail assessment consult (only $59 for those without extras private insurance).
Please feel free to book yourself in online or call our friendly Reception on (03) 8104 9270 today.
Ingrown Toenail Infection
Understand how you get ingrown toenails your self care home options and what you can do to get rid of them once and for all. You don't need to put up with the pain of an ingrown toenail any longer.

Bellevue Podiatry Health Care Treatment
Bellevue Podiatry has been serving the people of Rosanna and its surrounding suburbs for over 10 years. We have the qualifications, experience and education to effectively treat any lower limb condition or injury that requires expert podiatry care.